
Medicare patients claims must be filed no later than the end of the calendar year following the year in which the services were provided. In this article, I have mentioned everything you need to know about timely filing limit along with the timely filing limit of all major insurances in United States. Medicare (Cigna for Seniors): In accordance with Medicare processing rules, non-participating health care providers have 15 to 27 months to file a new claim. Dear Aetna Better Health provider, We want you to receive payment for care you’ve provided to Aetna Better Health members enrolled in the Health Choices and the CHIP programs. Also ask your accounts receivable team to follow up on claims within 15 days of claim submission. If insurance company allows electronic submission then submit claims electronically and keep an eye on rejections. To avoid timely filing limit denial, submit claims within the timely filing limit of insurance company.
#Aetna timely filing limit 2021 how to#
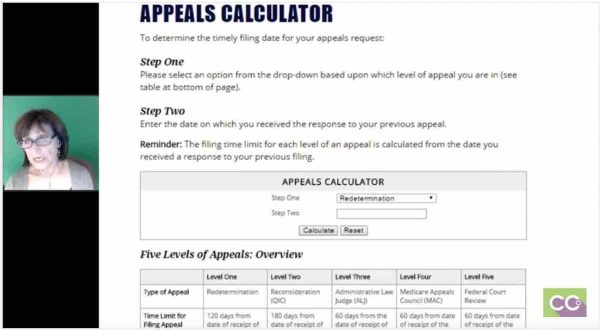
How to avoid from claim timely filing limit exhausted? All for an affordable and sometimes 0 plan premium. Texas Medicare Advantage plans often include prescription drug coverage and extra benefits. In situations where a claim was denied for not being filed timely, the provider has 180 calendar days from the date the denial was received from. What if claim isn’t sent within the timely filing limit?įailing to submit a claim within the timely filing limit may result in the claim being denied with a denial code CO 29, so it is important to be aware of the deadline and submit the claim promptly. Aetna Medicare Advantage plans in Texas are built to help you age actively. Unitedhealthcare Non Participating Providers Allow 15-days for electronic claims and 30 -days for paper claims before resubmitting. If filing electronically, be sure to also check your Availity® file acknowledgement and EBR for claim level failures. Keystone First Resubmissions & Corrected Claimsġ80 Calender days from Primary EOB processing dateġ2 months from original claim determination For claims status, use Availity® or contact Florida Blue. Amerigroup for Non Participating Providers


 0 kommentar(er)
0 kommentar(er)
